Post-traumatic stress disorder (PTSD) is a condition that can have a profound impact on the lives of those who experience it, particularly among veterans who have served in the armed forces. Not only does PTSD affect mental health, but it can also lead to the development of substance abuse problems. Understanding the relationship between PTSD and alcohol and other substance abuse is crucial to providing adequate support for these individuals and addressing their unique challenges. This article explores the connection between PTSD and substance abuse in veterans, as well as the consequences and available treatment options.
Understanding PTSD: An Overview
Post-traumatic stress disorder (PTSD) is a mental health condition that occurs as a result of experiencing or witnessing a traumatic event. It is a complex disorder that can have a profound impact on an individual’s life. Let’s delve deeper into the intricacies of PTSD and gain a better understanding of its symptoms and prevalence.

Defining PTSD and its Symptoms
PTSD is classified as a psychiatric disorder that occurs in response to a traumatic event. It is characterized by four main clusters of symptoms: intrusive thoughts, avoidance behaviors, negative mood and cognition, and hyperarousal.
Intrusive thoughts refer to re-experiencing traumatic events through flashbacks, nightmares, or distressing memories. These intrusive memories can be triggered by various stimuli, such as sights, sounds, or smells that remind the individual of the traumatic event. The vividness and intensity of these memories can be overwhelming, causing significant distress.
Individuals with PTSD often engage in avoidance behaviors as a coping mechanism. They may avoid specific places, activities, or people that may trigger memories of the traumatic event. This avoidance can lead to social isolation and a limited quality of life.

In addition, individuals with PTSD may experience negative changes in their thoughts and emotions. They may feel a persistent sense of guilt, shame, or self-blame for the traumatic event. These negative emotions can be debilitating and hinder their ability to engage in healthy relationships and activities.
Hyperarousal symptoms include an exaggerated startle response, difficulty sleeping, and constant feelings of being on edge. Individuals with PTSD may be hypervigilant, always scanning their environment for potential threats. This state of hyperarousal can be exhausting and make it challenging to relax or feel safe.
[ctabox]Are You or Someone You Know a Veteran Struggling with PTSD and Substance Abuse? We can Help[/ctabox]
The Prevalence of PTSD in Veterans
PTSD is not uncommon among veterans, particularly those who have been exposed to combat situations or other traumatic events during their military service. The nature of military service often exposes individuals to high-stress environments and life-threatening situations, increasing the risk of developing PTSD.
According to the U.S. Department of Veterans Affairs, approximately 11-20% of veterans who served in Operation Iraqi Freedom and Operation Enduring Freedom experience PTSD in a given year. These numbers highlight the significant impact that traumatic events can have on the mental well-being of our veterans.
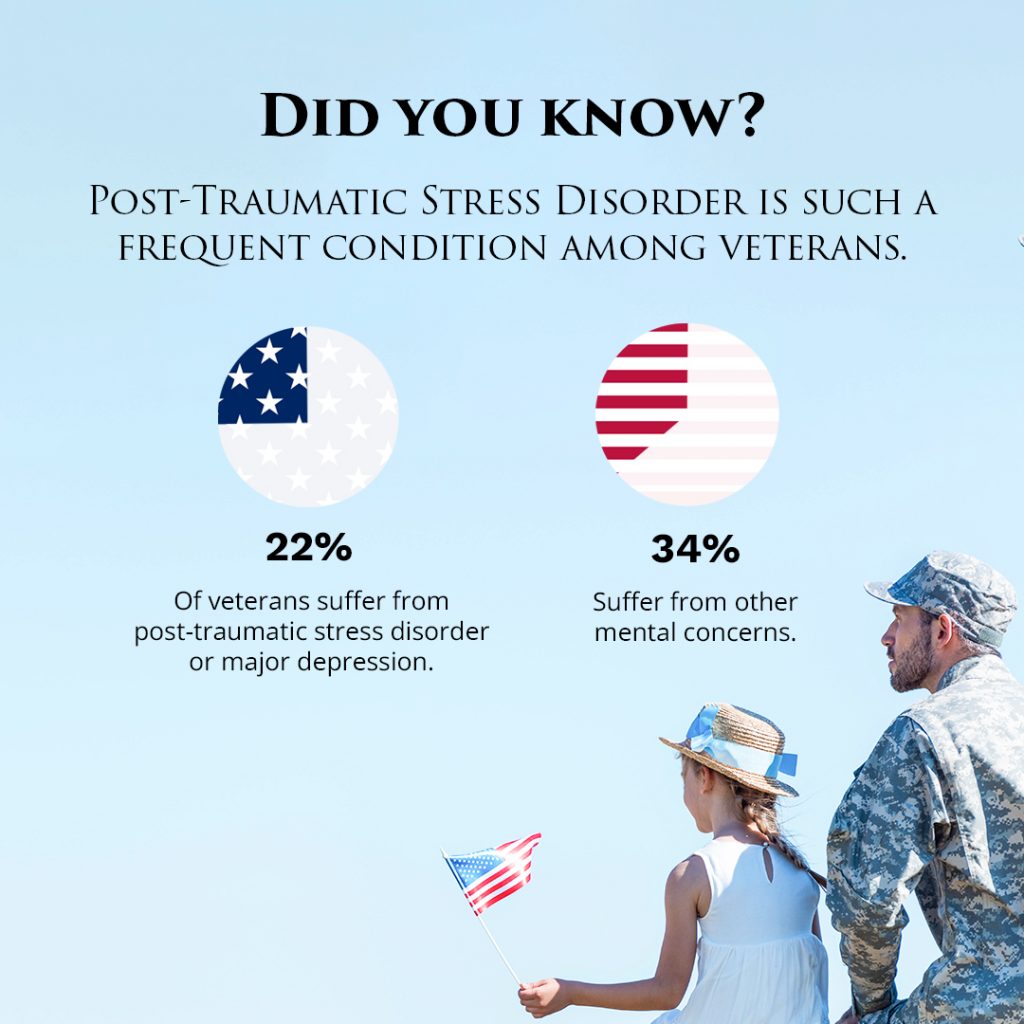
The prevalence of PTSD in veterans can vary depending on factors such as the intensity and duration of combat exposure. Those who have experienced multiple deployments or prolonged exposure to combat are at a higher risk of developing PTSD. It is crucial to provide adequate support and resources to help veterans cope with the psychological aftermath of their service.
It is important to recognize that PTSD is not limited to veterans. Anyone who has experienced or witnessed a traumatic event can develop this condition. By understanding the symptoms and prevalence of PTSD, we can work towards creating a more compassionate and supportive society for those affected by this debilitating disorder.
The Connection Between PTSD and Substance Abuse
The relationship between PTSD and substance abuse is complex and multifaceted. Many veterans with PTSD turn to substances as a means of self-medication or as a coping mechanism to alleviate the distressing symptoms associated with the disorder.
The Role of Self-Medication in PTSD
In an attempt to find relief from the emotional pain and distress caused by their PTSD symptoms, veterans may turn to substances such as alcohol or drugs. Self-medication refers to the use of substances to manage symptoms, even though it may not provide long-term relief or treatment for the underlying condition. Substances can temporarily numb emotional pain or help individuals escape from the intrusive thoughts associated with PTSD.

Substance Abuse as a Coping Mechanism
Substance abuse can also serve as a coping mechanism for veterans with PTSD. The addictive nature of drugs and alcohol can create a cycle of dependence, making it difficult for individuals to break free from the substance abuse pattern. Moreover, substance use may temporarily alleviate feelings of anxiety, depression, or insomnia associated with PTSD.
The Impact of Substance Abuse on Veterans with PTSD
When PTSD and substance abuse co-occur, the consequences can be particularly detrimental to veterans’ well-being. Substance abuse exacerbates the negative physical and mental health effects of PTSD, creating a vicious cycle that is challenging to overcome.
Physical Health Consequences
Substance abuse can have severe physical health consequences for veterans with PTSD. Excessive alcohol consumption, for example, can lead to liver damage, cardiovascular problems, and an increased risk of accidents. Drug abuse can also result in respiratory problems, compromised immune function, and cognitive impairment.

Mental Health Implications
The combination of PTSD and substance abuse can significantly worsen mental health outcomes for veterans. Substance abuse can intensify symptoms of depression, anxiety, and irritability, making it even more challenging to effectively manage the psychological effects of PTSD. Furthermore, the risk of suicide is notably higher in individuals with co-occurring PTSD and substance abuse.
Treatment Options for Veterans with PTSD and Substance Abuse
Addressing the dual diagnosis of PTSD and substance abuse requires an integrated approach that considers the unique needs of veterans. Effective treatment often involves a combination of therapy and medication interventions.
Therapy and Counseling Approaches
Cognitive-behavioral therapy (CBT) is highly effective in treating both PTSD and substance abuse. CBT helps individuals identify and challenge negative thought patterns, develop healthy coping strategies, and learn skills to manage cravings and avoid relapse.

In addition to CBT, other evidence-based therapy approaches such as eye movement desensitization and reprocessing (EMDR) and prolonged exposure therapy (PE) can be beneficial for veterans with PTSD. These therapies aim to reduce the distress associated with traumatic memories and promote healing.
Medication and Medical Interventions
Medication can be an essential component of the treatment plan for veterans with PTSD and substance abuse. Antidepressant medications such as selective serotonin reuptake inhibitors (SSRIs) may be prescribed to help manage symptoms of PTSD and address underlying depression or anxiety.
In cases where substance abuse is severe, detoxification and rehabilitation programs may be necessary to ensure a safe and supported recovery process. These programs typically include medically supervised withdrawal, counseling, and ongoing support to address both the physical and psychological aspects of addiction.
Prevention Strategies and Support Systems
Prevention strategies and strong support systems are crucial in mitigating the risk of substance abuse among veterans with PTSD.
Building Resilience in Veterans
By promoting resilience and providing tools to manage stress and develop healthy coping mechanisms, veterans can be better equipped to navigate the challenges associated with PTSD without turning to substances. Support programs that focus on resilience-building and stress-reduction techniques can make a significant impact in preventing substance abuse.

The Importance of a Strong Support Network
A robust support network is essential for veterans with PTSD and substance abuse. Friends, family, and fellow veterans can provide invaluable support, understanding, and encouragement throughout the recovery journey. Additionally, peer support groups and specialized rehabilitation programs that cater specifically to veterans can foster a sense of belonging and provide a safe space for individuals to share their experiences.
In conclusion, the link between PTSD and substance abuse in veterans is undeniable. Veterans with PTSD often turn to substances as a form of self-medication or coping mechanism, leading to a cycle of addiction and worsening mental and physical health. However, with the right treatment, support, and prevention strategies, recovery from co-occurring PTSD and substance abuse is possible. Society must recognize and address the unique challenges faced by veterans, providing them with the support they need to overcome these complex issues and lead fulfilling lives.
Top-Rated Dual Diagnosis Program for Veterans at CBH
At Compassion Behavioral Health, we are deeply committed to helping veterans navigate the intricate maze of PTSD and substance abuse. Our tailored veteran programs, which are designed specifically for the military community, focus on holistic healing. We believe that by addressing the mind, body, and spirit, we can pave a path to wellness that is both sustainable and transformative. Through individualized therapy, group sessions, and resilience-building workshops, our team works diligently to reignite the hope and strength within each veteran we serve. To learn more, call us or contact us today.



