Oxycodone is a powerful opioid medication commonly prescribed for pain relief. Understanding how long it stays in the body is crucial for various reasons, including medical treatment, drug testing, and the management of potential side effects. This comprehensive guide will delve into the factors affecting oxycodone’s duration in the system, detection methods, and relevant information for users and healthcare providers.
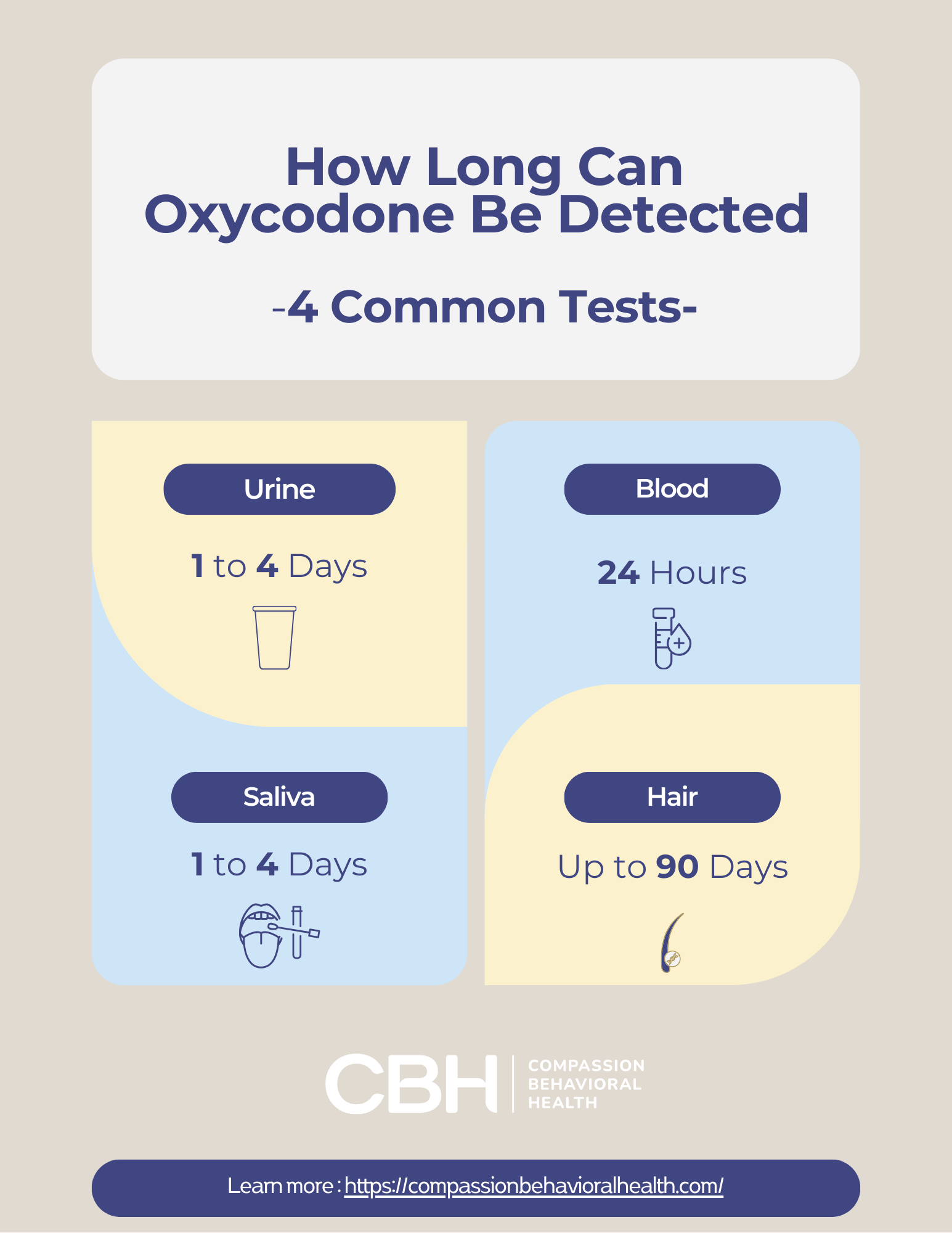
Oxycodone, a semi-synthetic opioid, is often prescribed for the management of moderate to severe pain. Understanding its pharmacokinetics is crucial, as it encompasses how the drug is absorbed, distributed, metabolized, and excreted in the body. In short, Oxycodone can be detected in urine for 1–4 days, blood for 24 hours, saliva for 1–4 days, and hair for up to 90 days. Detection time varies based on factors like dosage, frequency, metabolism, age, and overall health.The bioavailability of oxycodone can vary significantly based on the route of administration, with oral formulations generally having lower bioavailability compared to intravenous methods. This variability can lead to differences in efficacy and safety profiles, making it essential for healthcare providers to tailor prescriptions to individual patient needs while considering factors such as age, weight, and overall health status.
Moreover, the duration oxycodone remains detectable in the system can be influenced by numerous factors, including metabolic rate, frequency of use, and the presence of other substances in the body. For instance, individuals with slower metabolism may retain the drug longer, increasing the risk of potential side effects or overdose. Detection methods, such as urine tests, blood tests, and hair follicle analysis, each have their own timelines for how long oxycodone can be identified, which is critical information for both patients and healthcare professionals, especially in contexts such as pain management, substance abuse treatment, and legal situations.
Understanding Oxycodone
Oxycodone is an opioid analgesic used primarily to manage moderate to severe pain. It works by binding to specific receptors in the brain and spinal cord, altering the perception of pain and emotional response to it. While effective for pain relief, oxycodone also carries a risk of addiction and side effects. As a result, healthcare providers often weigh the benefits against potential risks when prescribing this medication, ensuring that it is used judiciously and monitored closely.
How Oxycodone Works
When ingested, oxycodone is metabolized in the liver and transformed into various active and inactive metabolites. The primary active metabolite, noroxycodone, contributes to its pain-relieving effects. The onset of action typically occurs within 30 minutes, with peak effects reached in about 1 to 2 hours. This rapid action makes oxycodone particularly useful in acute pain situations, where immediate relief is necessary. However, the duration of its effects can vary significantly based on individual metabolism, dosage, and whether it is taken in immediate-release or extended-release formulations.
Common Uses of Oxycodone
Oxycodone is prescribed for various conditions, including:
- Post-surgical pain
- Chronic pain conditions such as arthritis
- Severe headaches or migraines
- Cancer-related pain
In addition to these common uses, oxycodone may also be utilized in palliative care settings, where managing pain and improving quality of life for patients with terminal illnesses is paramount. Its versatility allows it to be tailored to individual patient needs, with dosages adjusted based on the severity of pain and patient response. Furthermore, oxycodone is often combined with other medications, such as acetaminophen or ibuprofen, to enhance its analgesic effects while minimizing the required dose of the opioid itself, thereby reducing the risk of side effects and dependency.
Despite its effectiveness, the use of oxycodone is closely monitored due to the potential for abuse and the development of tolerance. Patients are often advised about the importance of adhering to prescribed dosages and the risks associated with abrupt discontinuation, which can lead to withdrawal symptoms. Education on safe storage and disposal of unused medication is also crucial in preventing misuse, particularly in households with children or individuals at risk of substance abuse.
How Long Does Oxycodone Stay in Your System?
The duration oxycodone remains detectable in the body varies based on several factors. Generally, oxycodone can be detected in urine, blood, saliva, and hair, with each method having different detection windows. Understanding these detection times is crucial for individuals who may be subject to drug testing, whether for employment, legal reasons, or medical evaluations.
Detection Times by Method
The following outlines how long oxycodone can typically be detected in various bodily fluids:
- Urine: 1 to 4 days
- Blood: 24 hours
- Saliva: 1 to 4 days
- Hair: Up to 90 days
Factors Influencing Detection Duration
Several factors can influence how long oxycodone stays in the system, including:
- Dosage: Higher doses may take longer to clear.
- Frequency of Use: Chronic users may have longer detection times.
- Metabolism: Individual metabolic rates can vary significantly.
- Age and Health: Older adults and those with liver or kidney issues may metabolize oxycodone more slowly.
In addition to these factors, the method of administration can also play a role in how long oxycodone remains in the system. For instance, individuals who take oxycodone orally may experience different clearance times compared to those who use it intravenously. The route of administration affects how quickly the drug enters the bloodstream and how it is metabolized by the body. Furthermore, hydration levels can influence the concentration of oxycodone in urine; well-hydrated individuals may excrete the drug more quickly, potentially shortening detection times.
Another important aspect to consider is the potential for drug interactions. Certain medications can either speed up or slow down the metabolism of oxycodone, leading to variations in how long it stays detectable. For example, drugs that inhibit liver enzymes responsible for metabolizing oxycodone can prolong its presence in the system, while others that enhance these enzymes may facilitate faster clearance. This interplay between different substances highlights the complexity of drug metabolism and the importance of discussing all medications with a healthcare provider to understand their effects on oxycodone clearance.
Pharmacokinetics of Oxycodone
Pharmacokinetics refers to how the body absorbs, distributes, metabolizes, and excretes a drug. Understanding these processes is essential for determining how long oxycodone stays in the system.
Absorption and Distribution
Oxycodone is rapidly absorbed after oral administration, with bioavailability ranging from 60% to 87%. It is distributed throughout the body, with a volume of distribution of approximately 3 to 4 liters per kilogram. This means that oxycodone can reach various tissues, including the brain, where it exerts its analgesic effects. The rapid absorption contributes to its effectiveness in managing acute pain, making it a preferred choice in postoperative settings. Additionally, the drug’s ability to cross the blood-brain barrier allows it to provide relief from pain by binding to opioid receptors in the central nervous system, which can lead to both analgesia and euphoria, further influencing its potential for misuse.
Metabolism and Excretion
Oxycodone is primarily metabolized in the liver by enzymes, particularly CYP3A4 and CYP2D6. The metabolites are then excreted via urine. The half-life of oxycodone ranges from 3 to 5 hours, meaning that it takes this amount of time for half of the drug to be eliminated from the body. The metabolic pathways can vary significantly among individuals, influenced by genetic factors, age, and the presence of other medications. For instance, individuals with variations in the CYP2D6 enzyme may experience altered effects and side effects due to differences in how oxycodone is processed. Furthermore, the presence of liver or kidney impairment can lead to prolonged drug exposure, necessitating careful monitoring and potential dosage adjustments to avoid toxicity.
Implications for Drug Testing
Understanding how long oxycodone stays in the system is crucial for those undergoing drug testing, whether for employment, legal reasons, or medical evaluations. Different tests have varying sensitivities and detection windows, which can significantly impact the outcomes for individuals who may be using the medication legally or illegally.
Workplace Drug Testing
Many employers conduct drug tests to ensure a safe working environment. Oxycodone may be included in standard drug panels, particularly in industries where safety is paramount. Employees should be aware of the potential for false positives, especially if they are taking prescribed medications. It is essential for employees to communicate openly with their employers about any medications they are taking, as this can help mitigate misunderstandings and ensure that safety protocols are maintained without penalizing those who are compliant with medical advice.
Furthermore, the increasing prevalence of prescription drug use in the workplace has led to a growing need for employers to establish clear drug testing policies. These policies should not only address the substances being tested but also provide guidance on how to handle situations involving legitimate prescriptions. Training for supervisors and HR personnel on the nuances of drug testing and prescription medications can foster a more informed and compassionate workplace culture.
Legal and Medical Considerations
In legal situations, such as DUI cases, the presence of oxycodone can have serious implications. Legal professionals often need to navigate complex issues surrounding the legality of drug use, especially when it comes to prescription medications. The interpretation of drug testing results can vary widely, and individuals may find themselves facing severe penalties, including license suspension or incarceration, if oxycodone is detected in their system during a legal investigation.
Medical professionals may also need to consider drug testing results when prescribing medications or managing treatment plans for patients with a history of substance use. This consideration is particularly important in pain management, where oxycodone is frequently prescribed. Physicians must balance the need to alleviate pain with the responsibility to prevent potential misuse or dependency. Regular monitoring and open discussions about medication use can help ensure that patients receive the care they need while minimizing the risks associated with opioid medications.
Factors Affecting Individual Response to Oxycodone
Individual responses to oxycodone can vary widely. Factors such as genetics, overall health, and concurrent medications can influence how the drug is metabolized and its effects on the body.
Genetic Factors
Genetic variations can affect how individuals metabolize oxycodone. For example, some people may have a genetic predisposition that leads to faster or slower metabolism of the drug, impacting both its efficacy and duration in the system. This variability is largely due to polymorphisms in genes coding for enzymes involved in drug metabolism, such as the cytochrome P450 family. As a result, two individuals taking the same dose of oxycodone may experience vastly different pain relief or side effects, leading to challenges in finding the optimal dosage for effective pain management.
Health Conditions
Certain health conditions can also influence how oxycodone is processed. Individuals with liver or kidney disease may experience prolonged effects due to impaired metabolism and excretion. Additionally, those with respiratory issues may be at higher risk for complications related to opioid use. Chronic obstructive pulmonary disease (COPD) or sleep apnea can exacerbate the respiratory depressant effects of oxycodone, necessitating careful monitoring and possibly alternative pain management strategies. Furthermore, conditions such as obesity can alter drug distribution and metabolism, complicating the clinical picture and requiring healthcare providers to tailor their approach to each patient’s unique health profile.
Concurrent Medications
Another critical factor influencing an individual’s response to oxycodone is the use of concurrent medications. Certain drugs can interact with oxycodone, either enhancing its effects or increasing the risk of adverse reactions. For instance, benzodiazepines, commonly prescribed for anxiety or insomnia, can amplify the sedative effects of oxycodone, leading to heightened risks of respiratory depression and overdose. Conversely, some medications may inhibit the enzymes responsible for oxycodone metabolism, potentially leading to increased plasma levels and prolonged effects. It is essential for healthcare providers to conduct a thorough medication review to identify potential interactions and adjust treatment plans accordingly, ensuring patient safety while effectively managing pain.
Safe Use of Oxycodone
While oxycodone can be an effective pain management tool, it is essential to use it safely to minimize the risk of addiction and side effects. Patients should follow their healthcare provider’s instructions closely.

Dosage Guidelines
Oxycodone is available in various formulations, including immediate-release and extended-release. Dosage should be tailored to the individual’s needs, taking into account their pain level, medical history, and response to the medication.
Monitoring and Follow-Up
Regular follow-up appointments with healthcare providers are crucial for those taking oxycodone. These appointments allow for monitoring of effectiveness, side effects, and any potential signs of misuse or addiction.
Key Considerations for Safe and Informed Oxycodone Use
Understanding how long oxycodone stays in the system is essential for both users and healthcare providers. With a detection window that varies based on multiple factors, it is crucial to consider individual circumstances when assessing the implications of oxycodone use. By following prescribed guidelines and maintaining open communication with healthcare professionals, users can effectively manage their pain while minimizing risks associated with opioid medications.
In summary, oxycodone is a powerful medication that requires careful management. Awareness of its pharmacokinetics, detection methods, and individual factors can help ensure safe and effective use. Always consult with a healthcare provider for personalized advice and treatment options.
Opioid Addiction Treatment at CBH in Florida
If you or a loved one is navigating the complexities of oxycodone use, whether it’s concerning its duration in the system or seeking help for substance use disorders, Compassion Behavioral Health is here to offer the support and care you need. Our personalized opioid addiction treatment plans are designed to foster sustainable recovery and improved mental health. Located conveniently in South Florida, our Hollywood rehab center provides a serene environment conducive to healing. Don’t hesitate to take the first step towards reclaiming your life. Call Us Today and let us be the ray of hope on your journey to wellness.