In today’s fast-paced world, stress and trauma are unfortunately all too common. When experiencing a distressing event, it is natural for individuals to react in different ways. Some may develop Acute Stress Disorder (ASD), while others may develop Post-Traumatic Stress Disorder (PTSD). While these two conditions may share similarities, it is important to understand their differences in order to provide appropriate support and treatment. In this article, we will explore the definitions, symptoms, causes, and treatment options for both ASD and PTSD. We will also highlight the key differences between these conditions and delve into their impact on daily life. Let’s begin by understanding Acute Stress Disorder in more detail.
What is Acute Stress Disorder
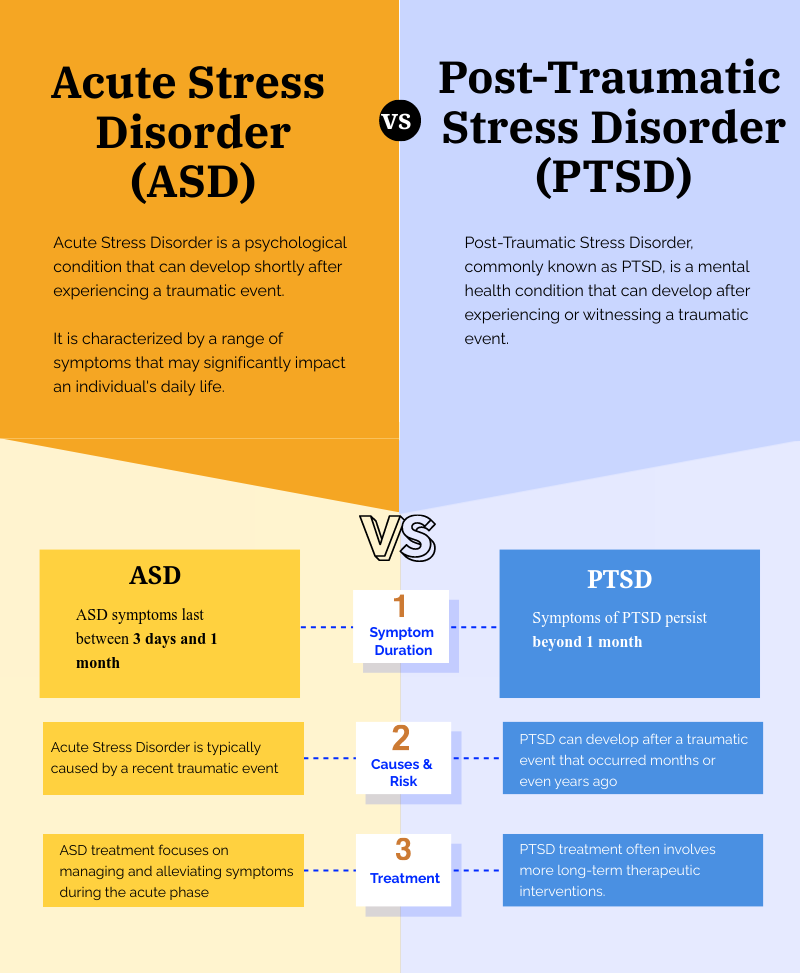
Acute Stress Disorder is a psychological condition that can develop shortly after experiencing a traumatic event. It is characterized by a range of symptoms that may significantly impact an individual’s daily life. These symptoms typically persist for a minimum of three days and can last for up to one month.
When someone goes through a traumatic event, their mind and body can be overwhelmed by the intensity of the experience. Acute Stress Disorder is a natural response to such events, as the individual’s brain tries to process and make sense of what happened. During this time, the person may feel a wide range of emotions, including fear, sadness, anger, and confusion.
Symptoms of Acute Stress Disorder
The symptoms of Acute Stress Disorder can vary from person to person. Individuals with Acute Stress Disorder may experience a range of symptoms that can be categorized into different groups:
- Intrusive Symptoms: Recurrent, involuntary memories, distressing dreams, or flashbacks related to the traumatic event. These memories can be triggered by seemingly innocuous stimuli, such as a particular sound or smell, which can transport the individual back to the moment of trauma.
- Avoidance Symptoms: Efforts to avoid reminders of the trauma, including people, places, or activities. This avoidance can lead to significant lifestyle changes, as individuals may withdraw from social interactions or stop engaging in activities they once enjoyed.
- Negative Mood: Feelings of detachment or inability to experience positive emotions. This emotional numbness can create a barrier to forming new relationships and enjoying life, leading to a sense of isolation.
- Hyperarousal Symptoms: Increased irritability, difficulty sleeping, or exaggerated startle response. Individuals may find themselves on edge, constantly anticipating danger, which can be exhausting and lead to further mental health complications.
Causes and Risk Factors of Acute Stress Disorder
Acute Stress Disorder is primarily caused by experiencing or witnessing a traumatic event such as a natural disaster, assault, or accident. The intensity and duration of the event, as well as an individual’s previous history of trauma, can influence the likelihood of developing ASD.
When a traumatic event occurs, the brain’s stress response system is activated, releasing hormones that prepare the body to fight, flee, or freeze. This response is essential for survival in dangerous situations, but when the event is overwhelming, it can lead to the development of Acute Stress Disorder.
Some risk factors that can increase the susceptibility to Acute Stress Disorder include:
- A history of previous trauma or childhood adversity.
- Lack of social support or a weak support system.
- Pre-existing mental health conditions such as anxiety or depression.
- Perceived lack of control or unpredictability during the traumatic event.
It is important to remember that everyone’s experience of trauma is unique, and not everyone who goes through a traumatic event will develop Acute Stress Disorder. Factors such as individual resilience, coping mechanisms, and access to support can also play a role in determining the impact of a traumatic event on an individual’s mental health.
Treatment Options for Acute Stress Disorder
Treating Acute Stress Disorder typically involves a combination of therapy and medication. The primary goal of treatment is to alleviate symptoms and help individuals regain control over their lives.
Cognitive-Behavioral Therapy (CBT) is a commonly used therapeutic approach for Acute Stress Disorder. This type of therapy helps individuals identify and challenge negative thought patterns and behaviors associated with the traumatic event. By working with a trained therapist, individuals can learn coping skills and strategies to manage their symptoms and reduce distress.
Another treatment option for Acute Stress Disorder is Eye Movement Desensitization and Reprocessing (EMDR). EMDR combines exposure therapy with lateral eye movements to help individuals process traumatic memories and reduce distressing symptoms. This therapy aims to reprocess the traumatic memories in a safe and controlled environment, allowing the individual to gain a new perspective and reduce the emotional intensity associated with the event.
In some cases, medication such as antidepressants or anti-anxiety medications may be prescribed to manage symptoms of Acute Stress Disorder. These medications can help regulate mood, reduce anxiety, and improve sleep quality. It is important to work closely with a healthcare professional to determine the most appropriate medication and dosage for each individual’s specific needs.
It is worth noting that recovery from Acute Stress Disorder is possible with the right support and treatment. With time and appropriate interventions, individuals can learn to cope with their symptoms, regain a sense of control, and move forward in their lives.
Understanding Post-Traumatic Stress Disorder
Post-Traumatic Stress Disorder, commonly known as PTSD, is a mental health condition that can develop after experiencing or witnessing a traumatic event. It is different from Acute Stress Disorder in terms of duration and timing.
Symptoms of PTSD
The symptoms of PTSD can be grouped into four main categories:
- Intrusion: Intrusive thoughts, nightmares, or flashbacks related to the traumatic event.
- Avoidance: Avoidance of places, people, or activities that remind the individual of the traumatic event.
- Negative Alterations in Mood and Cognition: Negative changes in thoughts, emotions, and beliefs about oneself or others.
- Hyperarousal: Persistent feelings of heightened alertness, irritability, and difficulty concentrating or sleeping.
Causes and Risk Factors of PTSD
PTSD can develop after experiencing or witnessing a wide range of traumatic events such as military combat, sexual assault, or serious accidents. Although anyone can develop PTSD, certain risk factors may increase an individual’s susceptibility:
- Intense or prolonged trauma.
- Personal history of trauma or previous mental health conditions.
- Lack of social support or limited coping mechanisms.
- High-stress levels in daily life.
Treatment Options for PTSD
Similar to Acute Stress Disorder, treatment for PTSD often involves a combination of therapy and medication. The primary goals of treatment are to reduce symptoms, improve overall functioning, and enhance quality of life.
Some common treatment options for PTSD include:
- Cognitive-Behavioral Therapy (CBT): This type of therapy aims to address and modify negative thought patterns and behaviors associated with the traumatic event.
-
Dialectical Behavioral Therapy (DBT): By gradually exposing individuals to the memories and sensations associated with the traumatic event, this therapy helps reduce avoidance symptoms.
- Medication: Selective serotonin reuptake inhibitors (SSRIs) and other antidepressant medications may be prescribed to alleviate symptoms of PTSD.
Diagnosis and Assessment
Diagnosing Acute Stress Disorder and PTSD involves a thorough assessment by a qualified mental health professional. Understanding the diagnostic criteria is essential for effective treatment. Early recognition of these disorders can significantly influence the recovery trajectory and overall well-being of individuals affected by trauma.
Diagnosis and Assessment
Diagnosing Acute Stress Disorder and PTSD involves a thorough assessment by a qualified mental health professional. Understanding the diagnostic criteria is essential for effective treatment. Early recognition of these disorders can significantly influence the recovery trajectory and overall well-being of individuals affected by trauma.
Diagnostic Criteria for Acute Stress Disorder
To be diagnosed with ASD, individuals must meet specific criteria outlined in the DSM-5, including:
- Exposure to a traumatic event.
- Presence of nine or more symptoms from the categories of intrusion, negative mood, dissociation, avoidance, and arousal.
- Symptoms lasting for three days to one month after the trauma.
It is important to note that the symptoms of Acute Stress Disorder can manifest in various ways, including intrusive memories, flashbacks, and heightened anxiety. These symptoms can disrupt daily functioning and lead to significant distress. Furthermore, individuals may experience dissociative symptoms, such as feeling detached from themselves or their surroundings, which can complicate their emotional response to the trauma. Recognizing these symptoms early on can facilitate timely intervention, which is crucial for preventing the progression to PTSD.
Diagnostic Criteria for PTSD
For PTSD, the criteria are more extensive and include:
- Exposure to a traumatic event.
- Presence of symptoms from four categories: intrusion, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity.
- Symptoms persisting for more than one month.
- Significant impairment in social, occupational, or other important areas of functioning.
Individuals diagnosed with PTSD may experience a range of symptoms that can severely impact their quality of life. Intrusive thoughts and nightmares can lead to sleep disturbances, while avoidance behaviors may result in social withdrawal and isolation. Additionally, negative alterations in cognition can manifest as persistent negative beliefs about oneself or the world, contributing to feelings of hopelessness and despair. The heightened arousal and reactivity can lead to irritability, anger outbursts, and hypervigilance, making it challenging for individuals to feel safe in their environments. Understanding these symptoms and their implications is vital for developing effective treatment plans that address the unique needs of each individual.
3 Key Differences Between Acute Stress Disorder and PTSD
1. Differences in Symptoms
While ASD and PTSD share similar symptoms, the key difference lies in their duration. ASD symptoms last between three days and one month, while symptoms of PTSD persist beyond one month. If symptoms continue for an extended period and significantly impair an individual’s daily life, a diagnosis of PTSD may be considered.
2. Differences in Causes and Risk Factors
Acute Stress Disorder is typically caused by a recent traumatic event, whereas PTSD can develop after a traumatic event that occurred months or even years ago. Additionally, the risk factors for developing these conditions can also vary, with ASD being more closely linked to the intensity and duration of trauma.
3. Differences in Treatment Approaches
The treatment approaches for ASD and PTSD are similar but may vary in intensity and duration due to the difference in symptom persistence. ASD treatment focuses on managing and alleviating symptoms during the acute phase, while PTSD treatment often involves more long-term therapeutic interventions.
The Impact of Acute Stress Disorder and PTSD on Daily Life
Effects on Personal Relationships
Both ASD and PTSD can have a significant impact on personal relationships. Individuals with ASD or PTSD may experience difficulties in expressing their emotions, connecting with others, and maintaining healthy relationships. Communication breakdowns and emotional distancing are common, making it crucial to provide support and understanding to those affected.
Effects on Work and Productivity
ASD and PTSD can also impact an individual’s ability to perform well at work. Concentration difficulties, sleep disturbances, and anxiety can contribute to decreased productivity and increased absenteeism. Creating a supportive work environment and offering accommodations can help individuals navigate their professional lives while managing their symptoms.
Effects on Mental and Physical Health
The toll of ASD and PTSD extends to one’s mental and physical well-being. The constant state of hypervigilance and emotional distress can lead to sleep disorders, weakened immune systems, and an increased risk of developing other mental health conditions such as depression and anxiety. Seeking appropriate treatment and practicing self-care are crucial for managing the long-term impact of these conditions.
While Acute Stress Disorder and Post-Traumatic Stress Disorder may share similarities, understanding their differences is essential for proper diagnosis and treatment. If you or someone you know is struggling with the aftermath of a traumatic event, seeking professional help can make a significant difference in one’s journey towards healing and resilience.
ASD and PTSD Treatment at CBH
At Compassion Behavioral Health, we are committed to providing comprehensive and individualized care for those dealing with the effects of trauma. Our team of mental health professionals understands the complexities of both Acute Stress Disorder (ASD) and Post-Traumatic Stress Disorder (PTSD) and is equipped to offer a range of therapies tailored to meet the unique needs of each individual.
We believe that recovery is a collaborative process, and we work closely with our clients to create a supportive and empowering environment. Our approach integrates evidence-based treatments with a deep understanding of the personal experiences and challenges faced by individuals with ASD and PTSD. Call us today to learn more about our evidence-based treatment program.



